File:Assessment and treatment algorithm for overweight and obesity.png
Assessment_and_treatment_algorithm_for_overweight_and_obesity.png (682 × 525 pixels, file size: 55 KB, MIME type: image/png)
| This free media file is from Wikimedia Commons. Its description page is included below. |
Summary
| DescriptionAssessment and treatment algorithm for overweight and obesity.png | |
| Date | 2 October 2010 (upload date) |
| Source | Page at National Heart, Lung, and Blood Institute at the U.S. Department of Health & Human Services |
| Author | National Heart, Lung, and Blood Institute |

|
This diagram image could be re-created using vector graphics as an SVG file. This has several advantages; see Commons:Media for cleanup for more information. If an SVG form of this image is available, please upload it and afterwards replace this template with
{{vector version available|new image name}}.
It is recommended to name the SVG file “Assessment and treatment algorithm for overweight and obesity.svg”—then the template Vector version available (or Vva) does not need the new image name parameter. |
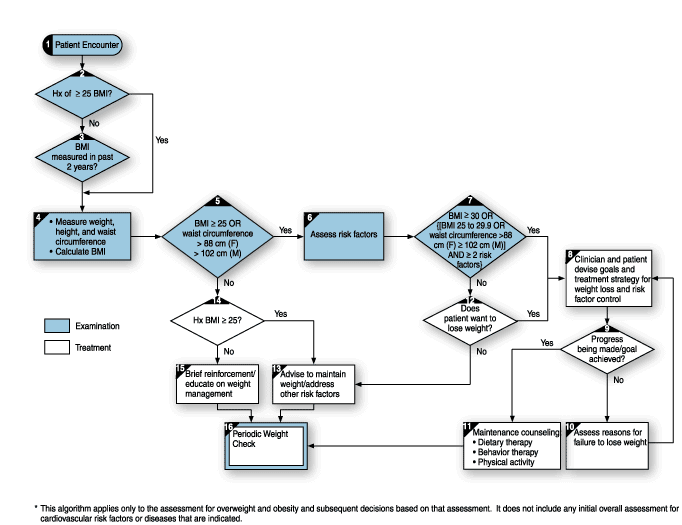
Algorithm description from source page
(This algorithm applies only to the assessment for overweight and obesity and subsequent decisions based on that assessment. It does not include any initial overall assessment for cardiovascular risk factors orf diseases that are indicated.)
Box 1: Patient Encounter
A patient encounter is defined as any interaction between a health care practitioner (generally a physician, nurse practitioner or physician's assistant) that provides the opportunity to assess a patient's weight status and provide advice, counseling, or treatment.
Box 2: History of Overweight or Recorded BMI greater than or equal to 25
The practitioner must seek to determine whether the patient has ever been overweight. While a technical definition is provided, a simple question such as "Have you ever been overweight?" will accomplish the same goal. Questions directed towards weight history, dietary habits, physical activities, and medications may provide useful information about the origins of obesity in particular patients.
Box 3: BMI Measured in Past 2 Years
For those who have not been overweight, a 2 year interval is appropriate for the reassessment of BMI. While this time span is not evidence-based, it is believed to be a reasonable compromise between the need to identify weight gain at an early stage and the need to limit the time, effort, and cost of repeated measurements.
Box 4: Measure, Weight, Height, Waist, Circumference; Calculate BMI
Weight must be measured so that the BMI can be calculated. Most charts are based on weights obtained with the patient wearing undergarments and no shoes. BMI can be manually calculated (kg/[height in meters]2), but is more easily obtained from a nomogram. Waist circumference is important because evidence suggests that abdominal fat is a particularly strong determinant of cardiovascular risk in those with a BMI of 25 to 34.9 kg/m2. Increased waist circumference can also be a marker of increased risk even in persons of normal weight. The technique for measuring waist circumference is described in the text. A nutrition assessment will also help to assess the diet and physical activity habits of overweight patients.
Box 5: BMI greater than or equal to 25, OR Waist Circumference 88 cm (35 in) or 102 cm (40 in)
These cut off points divide overweight from normal weight and are consistent with other national and international guidelines. The relation between weight and mortality is J-shaped, and evidence suggests that the right side of the "J" begins to rise at a BMI of 25. Waist circumference is incorporated as an "or" factor because some patients with BMI lower than 25 will have disproportionate abdominal fat, and this increases their cardiovascular risk despite their low BMI. These abdominal circumference values are not necessary for patients with a BMI greater than or equal to 35 kg/m2.
Box 6: Assess Risk Factors
Risk assessment for CVD and diabetes in a person with evident obesity will include special considerations for the history, physical examination, and laboratory examination. Of greatest urgency is the need to detect existing CVD or end-organ damage. Since the major risk of obesity is indirect (obesity elicits or aggravates hypertension, dyslipidemias, and diabetes, which cause cardiovascular complications), the management of obesity should be implemented in the context of these other risk factors. While there is no direct evidence demonstrating that addressing risk factors increases weight loss, treating the risk factors through weight loss is a recommended strategy.
Box 7: BMI greater than or equal to 30, OR ([BMI 25 to 29.9 OR Waist Circumference 88 cm (F) or 102 cm (M)] AND greater than or equal to 2 risk factors)
The panel recommends that all patients meeting these criteria attempt to lose weight. However, it is important to ask the patient whether or not they want to lose weight. Those with BMIs between 25 and 29.9 kg/m2 who have one or no risk factors should work on maintaining their current weight rather than embark on a weight reduction program. The panel recognizes that the decision to lose weight must be made in the context of other risk factors (e.g., quitting smoking is more important than losing weight) and patient preferences.
Box 8: Clinician and Patient Devise Goals
The decision to lose weight must be made jointly between the clinician and patient. Patient involvement and investment is crucial to success. The patient may choose not to lose weight but rather to prevent further weight gain as a goal. The panel recommends as an initial goal the loss of 10 percent of baseline weight, to be lost at a rate of 1 to 2lb/week, establishing an energy deficit of 500 to 1,000 kcal/day. For individuals who are overweight, a deficit or 300 to 500 kcal/day may be more appropriate, providing a weight loss of about ½ to 1 lb/week. Also, there is evidence that an average of 8 percent of weight can be lost in a 6-month period. Since the observed average 8 percent weight loss includes people who do not lose weight, an individual goal of 10 percent is reasonable. After 6 months, most patients will equilibrate (caloric intake balancing energy expenditure) and will require adjustment of energy balance if they are to lose more weight.
The three major components of weight loss therapy are dietary therapy, increased physical activity, and behavior therapy. Lifestyle therapy should be tried for at least six months before considering pharmacotherapy. In addition, pharmacotherapy should be considered as an adjunct to lifestyle therapy in patients with a BMI greater than or equal to 30 with no concomitant obesity-related risk factors or diseases, or for patients with a BMI greater than or equal to 27 with concomitant obesity-related risk factors or diseases. The risk factors or diseases considered important enough to warrant pharmacotherapy at a BMI of 27-29.9 are hypertension, dyslipidemia, CHD, type 2 diabetes, and sleep apnea. However, sibutramine, an FDA approved drug for long-term use, should not be used in patients with a history of hypertension, CHD, congestive heart failure, arrhythmia, or history of stroke. Certain patients may be candidates for weight loss surgery. Each component of weight loss therapy can be introduced briefly. The selection of weight loss methods should be made in the context of patient preferences, analysis of past failed attempts, and consideration of the available resources.
Box 9: Progress Being Made/Goal Achieved
During the acute weight loss period and at 6-month and 1-year follow up visits, the patients should be weighed, BMI calculated, and progress assessed. If at any time it appears that the program is failing, a reassessment should take place to determine the reasons. If pharmacotherapy is being used, appropriate monitoring for side effects is recommended. If a patient can achieve the recommended 10 percent reduction in body weight in 6 months to 1 year, this change in weight can be considered good progress. The patient can then enter the phase of weight maintenance and long term monitoring. It is important for the practitioner to recognize that some persons are more apt to lose or gain weight on a given regimen and that this phenomenon cannot always be attributed to degree of compliance. However, if significant obesity remains and absolute risk from obesity-associated risk factors remains high, at some point an effort should be made to reinstitute weight loss therapy to achieve further weight reduction. Once a limit of weight loss has been obtained, the practitioner is responsible for long-term monitoring of risk factors and for encouraging the patient to maintain a reduced weight level.
Box 10: Assess Reasons for Failure to Lose Weight
If a patient fails to achieve the recommended 10 percent reduction in body weight in 6 months or 1 year, a reevaluation is required. A critical question is whether the level of motivation is high enough to continue clinical therapy. If motivation is high, revise the goals and strategies. If motivation is not high, clinical therapy should be discontinued, but the patient should be encouraged to embark on efforts to lose weight or to at least avoid further weight gain. Even if weight loss therapy is stopped, risk factor management must be continued. Failure to achieve weight loss should prompt the practitioner to investigate energy intake (dietary recall including alcohol intake, daily intake logs), energy expenditure (physical activity diary), attendance at behavior therapy group meetings, recent negative life events, family and societal pressures, or evidence of detrimental psychiatric problems (depression, binge eating disorder). If attempts to lose weight have failed, and the BMI is greater than or equal to 40, surgical therapy should be considered.
Box 11: Maintenance Counseling
Evidence suggests that over 80 percent of persons who lose weight will gradually regain it. Patients who continue on weight maintenance programs have a greater chance of keeping weight off. Maintenance consists of continued contact with the health care practitioner for continued education, support, and medical monitoring.
Box 12: Does the Patient Want to Lose Weight?
All patients who are overweight (BMI 25 to 29.9) or do not have a high waist circumference, and have few (0 to 1) cardiovascular risk factors and do not want to lose weight, should be counseled regarding the need to keep their weight at or below its present level. Patients who wish to lose weight should be guided per Boxes 8 and 9. The justification for offering these overweight patients the option of maintaining (rather than losing) weight is that their health risk, while higher than that of persons with a BMI 25, is only moderately increased.
Box 13: Advise to Maintain Weight/Address Other Risk Factors
Those who have a history of overweight and are now at appropriate weight, and those who are overweight and not obese but wish to focus on maintenance of their current weight, should be provided with counseling and advice so that their weight does not increase. An increase in weight increases their health risk and should be prevented. The physician should actively promote prevention strategies including enhanced attention by the patient to diet, physical activity, and behavior therapy. For addressing other risk factors, see Box 6, because even if weight loss cannot be addressed, other risk factors should be covered.
Box 14: History of BMI greater than or equal to 25
This box differentiates those who are not overweight now and never have been from those with a history of overweight. See Box 2
Box 15: Brief Reinforcement
Those who are not overweight and never have been should be advised of the importance of staying in this category.
Box 16: Periodic Weight, BMI, and Waist Circumference Check
Patients should receive periodic monitoring of their weight, BMI, and waist circumference. Patients who are not overweight or have no history of overweight should be screened for weight gain every 2 years. This time span is a reasonable compromise between the need to identify weight gain at an early stage and the need to limit the time, effort, and the cost of repeated measurements.
Licensing
| Public domainPublic domainfalsefalse |
This image is a work of the Centers for Disease Control and Prevention, part of the United States Department of Health and Human Services, taken or made as part of an employee's official duties. As a work of the U.S. federal government, the image is in the public domain.
eesti ∙ Deutsch ∙ čeština ∙ español ∙ português ∙ English ∙ français ∙ Nederlands ∙ polski ∙ slovenščina ∙ suomi ∙ македонски ∙ українська ∙ 日本語 ∙ 中文(简体) ∙ 中文(繁體) ∙ العربية ∙ +/− |
Captions
Items portrayed in this file
depicts
image/png
28211d0a219367e1decac2054a304b7b34e6e222
55,948 byte
525 pixel
682 pixel
File history
Click on a date/time to view the file as it appeared at that time.
| Date/Time | Thumbnail | Dimensions | User | Comment | |
|---|---|---|---|---|---|
| current | 06:47, 2 October 2010 |  | 682 × 525 (55 KB) | Mikael Häggström | {{Information |Description={{en|1=Assessment and treatment algorithm for overweight and obesity. ==Algorithm description from source page== (This algorithm applies only to the assessment for o |
File usage
The following page uses this file:
Global file usage
The following other wikis use this file:
- Usage on ar.wikipedia.org
- Usage on bg.wikipedia.org
- Usage on bs.wikipedia.org
- Usage on en.wikipedia.org
- Usage on es.wikipedia.org
- Usage on fa.wikipedia.org
- Usage on ja.wikipedia.org
- Usage on ru.wikipedia.org